‘Sticks and stones may break my bones, but names will never hurt me’. A phrase we were often told as children? Something we try and tell ourselves is true? In an ideal world – yes. But in reality, other people’s opinions of us and the things they say or do can be hurtful and have a huge impact on the way we feel, the way we see ourselves and the way we live our lives.
Life really can be a rollercoaster – a series of ups, downs, and every emotion from jubilation to fear. The problem is – sometimes the downs seem to last longer and hit harder. Difficulty in just one aspect of life can have a huge impact on every other aspect of, not just your life, but those of the people around you.

Previously I wrote about work related stress. This is something I experienced myself. I was working 65 plus hours per week in supposedly a part time role, giving my heart and soul to my work. Yet I was constantly told that I was not doing enough, wasn’t meeting targets and could be doing better. I was spoken to in a tone that made me feel inferior and was subjected to tuts and eye rolls on a regular basis. It hit me hard. Being a teacher was not just a job, it was a part of who I was as a person. I had enjoyed a successful career of 15 years, I had progressed to a senior position in the school where I worked and had had a positive impact on many young lives. That all changed rapidly when new management stepped in and slowly and painfully ripped every ounce of confidence I ever had away from me.
When people behave negatively towards you and criticise you enough times, you slowly begin to believe what they are saying is true. Are people entitled to their opinions? Absolutely. Should we be open to constructive criticism and seek to always improve and develop? Most definitely. But should we have to listen to people, who are supposed to be professionals, speak down to us like a piece of dirt on their shoe? Be negative towards us, without opportunity to respond with a differing point of view? Make personal comments to our faces and behind our backs? Belittle us in front of colleagues, other professionals, children and parents? No, never! Unfortunately though, this is a reality. Some people think they have the right to say whatever they like, whenever they like and to whoever they like, with a total disregard for how it makes that person feel. In my case, this was what I had to put up with from my superiors at work. But it is by no means unique to me, or a workplace situation. It could be:
– Parents
– A partner/spouse
– Friends
– Work colleagues/ fellow students
– Family
– People we meet out and about/ speak to online
Or any number of other situations. Essentially, it can be anyone we interact with. It could be one, throwaway comment or an ongoing cycle of behaviour.
Over time, those negative feelings, attitudes and/or words are imbedded and it is quite likely as a result to become self-critical of everything. It’s then a vicious cycle – if you don’t believe in yourself, who else is going to believe in you. If you don’t think you can do something well, you won’t. If you behave negatively, you will more likely receive more negativity. It’s a downward spiral that spills out from one situation and begins affecting other aspects of day to day life.

So how does this negative behaviour affect us?
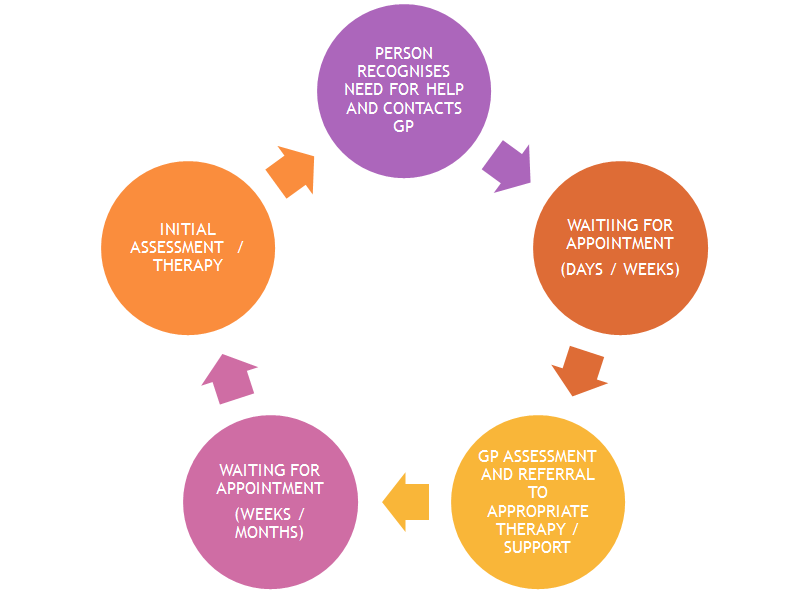
For me, I started shutting myself off from the world. I felt like a burden – useless and worthless. I carried on with day to day living but I often felt like a zombie, going through the motions. I hated myself and couldn’t see why anyone wanted to be around me. I felt that if people were kind to me or tried to spend time with me it was because they felt like they should, not because they actually wanted to. When things were really bad, I would lie in bed wondering how I could make myself ill so I didn’t have to leave the house, and I considered crashing my car on the way to work so I didn’t have to go in. My GP suggested I access counselling to try and understand how I was feeling and try to rebuild my confidence. But I was warned that there was a long waiting list to access NHS counselling sessions. I didn’t see myself as a priority, I thought there were many people more in need than me, so I didn’t even put my name down. I wish I had done. Or, I wish I had known then what I know now – that there are many options out there that don’t require going via the NHS and your GP.
Thankfully, I am one of the lucky ones. I have an amazing husband, who stood by me every step of the way. I have two wonderful children that gave me a reason to keep going every day. And I have a supportive family and circle of close friends who stuck by me and have helped me come out of the other side. I don’t really know what was ‘wrong’ with me. Was I depressed? Was I suffering from anxiety? Was I stressed? I don’t really know. I just know I was in a very deep hole and for quite a while, I had no idea how to get out.
So how did I get out? What steps can be taken to get out of a situation like this?
– Try to remove yourself from the negativity (For me this meant leaving my job)
– Talk to someone about how you feel (Family, friends, a professional)
– Accept support from the people who care about you (If they are still there it is because they want to be)
– Acknowledge the positive aspects of your life (There will be some, find them)
– Try not to compare yourself or your situation to others (You are the only you – the one that matters)
– Try to look to the future, set yourself some goals (However tiny they may be at first)
When I reflect on this difficult time in my life… I hate that my children saw me break down in tears on numerous occasions. I’m sad that I feel like I lost over a year of my life to this. I am angry that my career was ripped from me, by those people who should have been supporting and guiding me. I feel guilty that so many people were affected by me being down, angry, upset, unsociable and generally negative. But I am trying to move forward positively and see the good that has come from it too. I am thankful that I am surrounded by people that care about me and that want to be around me. I am optimistic that if I can get through the last 12 months relatively unscathed then I can get through pretty much anything. I am excited that I have a new job, working with some really great people, on a project that could make a huge difference to a vast amount of people. I am eager to promote mental health awareness, encourage people to talk about how they feel and access help when needed.

I managed to fight myself out of that dark place. If you feel lost, alone, sad, angry, empty, worthless, like you are stuck in a rut – you can get out of it too. There is no need to tackle difficult times by yourself. Yes, friends and family are amazing, if you are lucky enough to have them around you. But mental health professionals are exactly that – they are the experts in guiding you through difficult times.
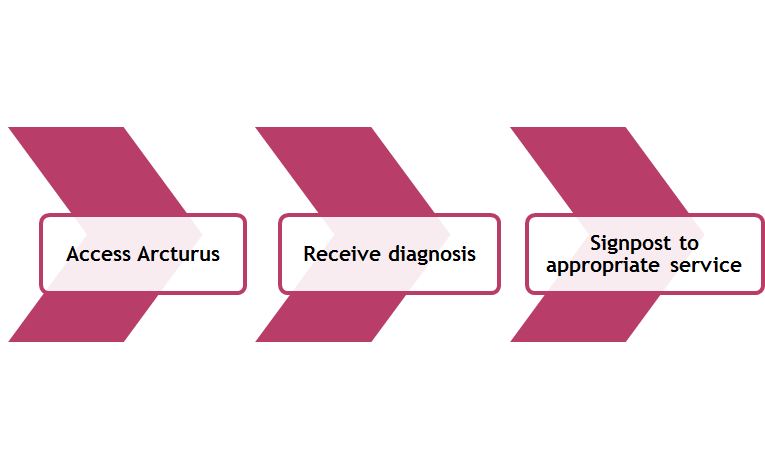
The help is out there and if you don’t know where, then use this online directory to find support near you … https://solis.directory
By Lisa French, Psychological Assistant